The Transformative Impact of Point-of-Care Ultrasound (POCUS)
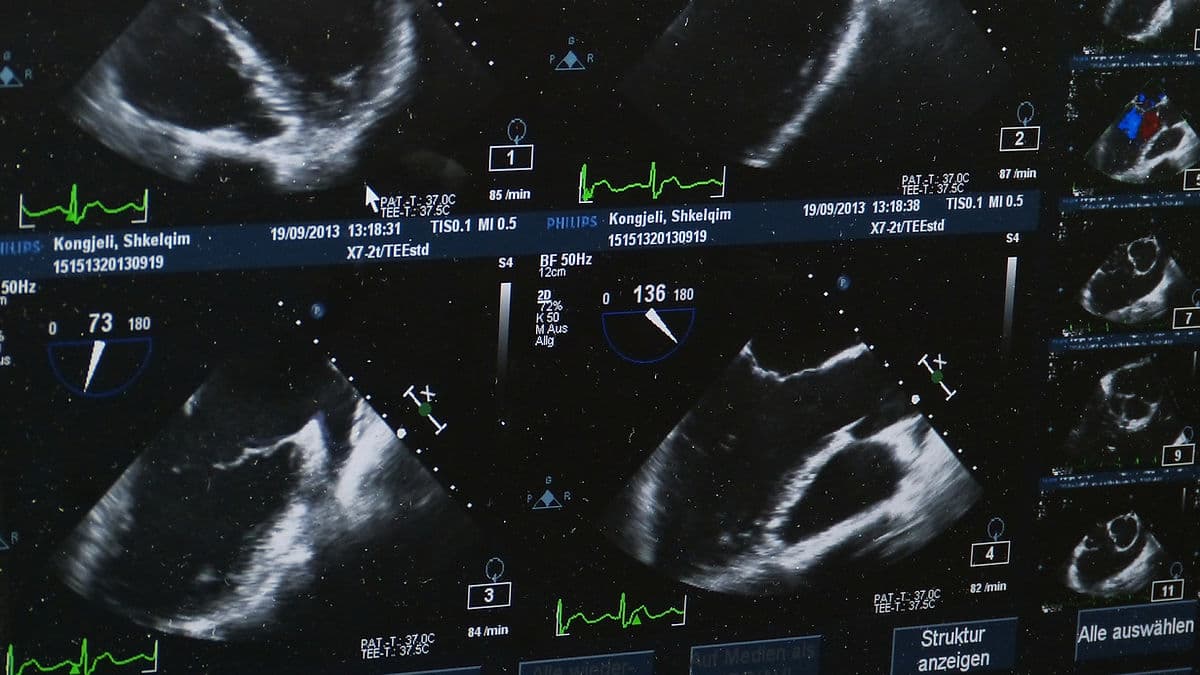
Point-of-Care Ultrasound (POCUS) has transformed the way clinicians assess and manage patients in real time. It brings diagnostic imaging directly to the bedside, shifting away from traditional radiology suites. Ultrasound has become an essential extension of the physical exam. This technology empowers healthcare providers with instant, actionable data. Whether in the emergency department, ambulance, or ICU, POCUS enhances clinical decision-making. It expedites treatment and, ultimately, improves patient outcomes. Its capability to provide immediate and dynamic imaging has redefined the standard of care, making it an indispensable skill for modern healthcare professionals.

What is POCUS?
POCUS refers to the use of portable ultrasound devices at the patient's bedside. This technology answers specific clinical questions in real-time. Unlike traditional ultrasound examinations performed in dedicated imaging departments, POCUS integrates seamlessly into the clinical evaluation. Clinicians can correlate the imaging results with the patient’s symptoms and physical findings instantly. This immediacy facilitates rapid decision-making, which is crucial in emergency and critical care settings.
Scope and Applications of POCUS

POCUS can be implemented across various medical disciplines. In emergency medicine, the ICU, and pre-hospital settings, rapid, real-time imaging can make the difference between life and death. For instance, in the emergency department (ED), ultrasound aids in trauma assessment. It guides interventions such as chest tube placements and evaluates cardiac function in hemodynamically unstable patients. Additionally, it helps detect free fluid in cases of internal bleeding.
In the intensive care unit (ICU), POCUS plays a critical role in monitoring critically ill patients. It assesses fluid status, guides resuscitation efforts, and identifies life-threatening conditions, such as pneumothorax or cardiac tamponade. On the scene of an accident, first responders and emergency personnel can utilize portable ultrasound devices. They can quickly assess internal injuries, identify potential shock states, and make informed transport decisions. The portability, speed, and accuracy of POCUS make it invaluable in high-stakes environments requiring immediate clinical decisions.
Imaging Protocols in POCUS
POCUS relies on standardized protocols that ensure consistent, accurate, and rapid assessments in critical situations. Four widely used protocols are as follows:
1. FAST (Focused Assessment with Sonography for Trauma)
FAST is a rapid bedside ultrasound exam used in trauma settings to detect free fluid in the peritoneal, pericardial, and pelvic cavities. It provides essential information in unstable trauma patients, allowing for quick decision-making regarding surgical intervention.
Sonographic Views & Images Acquired:
- Right Upper Quadrant (RUQ) – Morison’s Pouch
- Purpose: Detects free fluid between the liver and kidney.
- Indicator of Injury: Anechoic fluid in Morison’s pouch may suggest hemoperitoneum.
- Left Upper Quadrant (LUQ) – Splenorenal Recess
- Purpose: Detects free fluid between the spleen and kidney.
- Indicator of Injury: Anechoic fluid in the splenorenal recess may indicate hemoperitoneum.
- Pelvic View – Pouch of Douglas
- Purpose: Detects free fluid in the lowest part of the abdomen.
- Indicator of Injury: Free fluid suggests intraperitoneal bleeding.
- Subxiphoid or Parasternal Long View – Pericardial Assessment
- Purpose: Identifies pericardial effusion or cardiac tamponade.
- Indicator of Injury: Anechoic fluid around the heart suggests hemopericardium, indicating potential cardiac tamponade.
2. eFAST (Extended Focused Assessment with Sonography for Trauma)
eFAST is an extension of the FAST exam. It incorporates lung views to assess for pneumothorax in trauma patients. This protocol quickly identifies free fluid and air abnormalities, critical in both blunt and penetrating trauma.
Sonographic Views & Images Acquired:
- Same views as FAST, plus:
- Lung Views – Pneumothorax Assessment
- Purpose: Identifies lung sliding or its absence.
- Indicator of Injury: Absent lung sliding suggests pneumothorax.
If free fluid or pneumothorax is detected, immediate communication with the trauma team is vital.
3. RUSH (Rapid Ultrasound for Shock and Hypotension)
The RUSH exam evaluates the heart, inferior vena cava (IVC), Morison's pouch, aorta, and lungs. Its primary aim is to determine the cause of hypotension and shock using the “Pump, Tank, Pipes” approach.
Pump (Heart): Evaluates cardiac function.
Tank (Intravascular Volume Status): Assesses IVC and peritoneal spaces.
Pipes (Vascular System): Examines large vessels for aneurysm, DVT, or obstruction.
4. BLUE (Bedside Lung Ultrasound in Emergency)
The BLUE protocol focuses on assessing lung sliding, B-lines, consolidations, and pleural effusions. This is essential for evaluating acute respiratory failure.
Sonographic Views & Images Acquired:
- Anterior Chest – Upper and Lower Blue Points
- Purpose: Identify lung sliding and assess for conditions such as pulmonary edema or pneumonia.
- Findings help differentiate causes of respiratory distress.
Diagnostic Targets of POCUS
POCUS is used to detect a variety of conditions, such as:
Cardiac: Pericardial effusion, cardiac tamponade, ventricular dysfunction.
Pulmonary: Pneumothorax, pleural effusion, pulmonary edema.
Abdominal: Free intraperitoneal fluid in trauma, ruptured abdominal aortic aneurysm (AAA).
Vascular: Deep vein thrombosis (DVT) and ultrasound-guided vascular access.
Importance and Benefits of POCUS
The incorporation of POCUS into clinical practice offers numerous benefits:
Enhanced Diagnostic Accuracy: POCUS improves physical examination findings, leading to more precise diagnoses.
Immediate Clinical Decision-Making: Real-time imaging allows for prompt interventions, essential in acute settings.
Procedure Guidance: POCUS increases the safety and success rates of various bedside procedures.
Patient Safety: By minimizing the need for patient transport and exposure to ionizing radiation, POCUS enhances patient safety.
Responding to Critical Findings
When emergency personnel or a sonographer identifies a critical finding during a POCUS examination, immediate action is essential:
Communicate Promptly: Inform the clinical team to facilitate swift clinical decisions.
Document Thoroughly: Record findings thoroughly, including images and measurements, for clinical correlation and future references.
Assist in Management: Be prepared to aid in any immediate interventions required based on findings.
Timely communication ensures that critical findings translate into appropriate and rapid patient care interventions.
Conclusion
POCUS represents a transformative advancement in patient care. It provides immediate, bedside diagnostic capabilities that supplement clinical assessment and decision-making. Utilizing POCUS protocols expands the toolset of healthcare providers and enhances patient outcomes. Embracing ongoing education and training in POCUS will allow healthcare professionals to harness its full potential in today’s evolving medical landscape.
Want to learn more? Check out the POCUS segment of our Abdomen Webinar Series! This session explores POCUS applications in emergency medicine, covering trauma assessments and critical care scenarios.
🔗 Explore our video series and more at www.prepry.com!

References:
American College of Emergency Physicians. (2019). ACEP policy statement: Emergency ultrasound guidelines. Annals of Emergency Medicine, 74(3), 470-482. https://www.acep.org/siteassets/new-pdfs/policy-statements/ultrasound-guidelines--emergency-point-of-care-and-clinical-ultrasound-guidelines-in-medicine.pdf
Fraleigh, C. D. M., & Duff, E. (2022). Point-of-care ultrasound: An emerging clinical tool to enhance physical assessment. The Nurse practitioner, 47(8), 14–20. https://doi.org/10.1097/01.NPR.0000841944.00536.b2
Lichtenstein, D. A. (2016). Lung ultrasound in the critically ill: The BLUE protocol. Springer. https://link.springer.com/book/10.1007/978-3-319-15371-1
Perera, P., Mailhot, T., Riley, D., & Mandavia, D. (2010). The RUSH exam: Rapid Ultrasound in Shock in the evaluation of the critically ill. Emergency medicine clinics of North America, 28(1), 29–vii. https://doi.org/10.1016/j.emc.2009.09.010
Rose, J. S., Bair, A. E., Mandavia, D., & Kinser, D. J. (2001). The FAST is not enough: Identifying patients with major torso trauma using the extended FAST (eFAST) examination. Journal of Trauma and Acute Care Surgery, 50(3), 476-479. https://doi.org/10.1097/00005373-200103000-00019
Shen-Wagner, J., & Deutchman, M. (2020). Point-of-care ultrasound: A practical guide for primary care. Family Practice Management, 27(6), 33-40.
Prepry Team
Sonography Educators & Exam Prep Experts